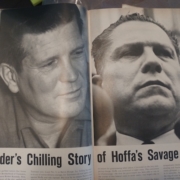
A Partin History
I’ve always found it difficult to write a memoir of my Partin family. Most of what I’ve written is publicly available, but few people outside of the FBI have put together pieces of the puzzle about my grandfather, Edward Grady Partin. You may already know about him, even if you don’t recall his name.
Read more